Trans Persons With Disabilities Lack Enabling Social Systems and Healthcare Support

India has laws and support systems for both transgender persons and people with disabilities, but none for those who are both identities – trans persons with disabilities. This shortcoming is felt most acutely in healthcare.
Kiran Nayak, a trans and disability rights activist, decided at age 31 to undergo gender affirmation surgery. Born with female organs, he said he grew up “with feelings of disgust about my own body”. But when he approached a hospital for the surgery, the medical staff questioned him about his choice – why would he want surgery when he was living with a disability? Nayak, whose mobility was impaired by early childhood polio, is a wheelchair user.
He recalled being hurt by the response, unable to see any link between his gender identity and his disability. “Medical systems complicate things for trans and disabled persons,” said Nayak, a trans man.
The activist runs two groups focused on trans and disability issues – the Karnataka Vikalachetanara Sanghatane and the Society for Transmen Action and Rights group (STAR) based in Andhra Pradesh and Telangana. His own research has brought him in touch with at least 17 persons with disabilities who identify as transgender persons in India. But this number could be a significant underestimation because of the challenges of coming out, he pointed out. Further, the government of India only identifies two genders — cis male and cis female — for the disability census.
In interviews with Behanbox, trans persons who live with disabilities complained that the medical fraternity is patronising and insensitive towards their healthcare needs. It does not help that families, already struggling to cope with their disability, find it hard to come to terms with their gender identity.
Lakshmikant, a 30-year-old from Telangana, has not been able to tell his parents that he has been living as a transman for the past several years. Speaking to them about gender affirmation surgery is unthinkable for him at the moment. “Because of my disability, they never considered that I had any feelings or felt any desires about living in and with my body,” he said.
Laws to protect the rights of the LGBTQI community and disabled persons, both fall under the ambit of the Ministry of Social Empowerment and Justice, but they are never seen together on an integrated platform. “In India, while we continue to witness significant mobilisations by the LGBTQI+ & disability rights movement, we have rarely seen these working closely with each other,” said Shampa Sengupta, an activist working on gender and disability issues, writing for Feminism in India.
As we reported earlier (here, here and here) transpersons have to constantly deal with discrimination, harassment and denial of care. But those who are also disabled end up being pushed even further into the margins, and struggle with anxieties and challenges on many more fronts – healthcare, social, familial and economic, among others.
“Across states, there are a significant number of trans persons with disabilities who are living in government facilities and have been beneficiaries of disability-related schemes. They feel if they reveal their trans identity, the staff will be un-accepting and they may be deprived of the basic facilities,” said Vyjayanti Vasanta Mogli, a transwoman and a Right to Information (RTI) activist.
An equitable model of public service distribution cannot leave anyone behind and the rights of trans persons, who now have legal recognition, should have equal access to health services, said Aqsa Shaikh, a trans woman and an associate professor of community medicine at Hamdard Institute of Medical Science and Research.
Skewed perception
Trans persons with disabilities run into challenges every step of the way in their search for healthcare, but their troubles start with social attitudes, say activists and community medicine experts.
“When you talk about trans persons with disabilities, the barriers in access start before reaching the hospital itself: for instance, lower levels of education, income and marginalisation. A lot of trans persons with disabilities may have left their homes because of the non-acceptance of their trans identity. Their identity documents may not be in their chosen names or pronouns,” said Harikeerthan Raghuram, project coordinator, Sangath, a not-for-profit organisation focused on community health among marginalised communities. “These barriers delay access to healthcare or [cause trans persons with disabilities to be] hesitant to [seek] access healthcare. They also cause a lot of mental distress.”
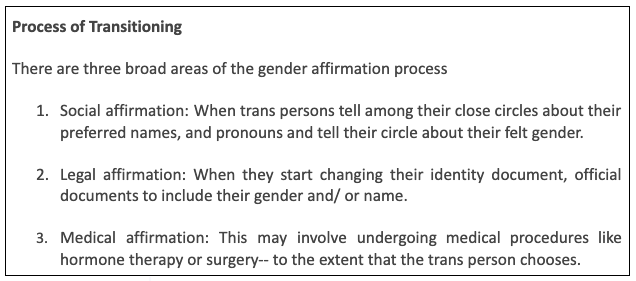
Healthcare providers’ lack of knowledge and confidence in addressing the gender identity of their trans patients, especially those with disabilities, can impact all potentially supportive interactions, said health activists. This is especially the case when a patient is transitioning.
“There has also been a historical pathologisation [viewing someone or something as ‘abnormal’] and that contributes to how trans and disabled patients are looked at by healthcare workers and that adds to the stigma,” said Aqsa Shaikh. “For people with disabilities, it starts with infrastructural barriers. For trans persons, there is no gender-neutral washroom, wards or changing rooms, which is a significant barrier.”
Troubles start at the gate
In November last year, Nayak fainted from extreme exhaustion and was rushed to a hospital by his wife. During the physical examination, the doctor asked him about the scars left by the gender affirmation surgery on his upper body.
“Most times trans people with disabilities cannot openly talk about their health issues with doctors and often doctors themselves are hesitant about or averse to touching us for a diagnosis. We need a safe space to talk about our intimate health problems,” said Nayak.
The trouble, says Sangath’s Raghuram, starts the moment someone like Nayak arrives at a medical facility. “Once they [trans people with disabilities] reach a hospital, the problem starts [at the gate] with the watchman, at the registration counter, in the queues – places where everything is mostly in the binary of male and female and everyone has their own biases and stigma,” said Raghuram. “Further, most hospitals are not disability-accessible – even the All India Institute of Medical Sciences (AIIMS) in Delhi.”
Rina*, a transwoman, reported a troubling experience with doctors. She has been diagnosed with schizophrenia and is also a bilateral below-knee amputee with two fingers missing in the right hand. Visits to doctors are traumatising, she said, because every time she mentions that she is on antipsychotics and other medicines for schizophrenia, they either infantilise her or address only her parents.
All doctors refuse to accept that she is a trans person. “They fed my parents this idea that I ‘think’ I am a woman because of schizophrenia,” said Rina.
Accessing psychiatric help is not easy for trans persons especially if families are not supportive or simply unaware, said Laxmikant. “Psychiatrists often refuse to give a diagnosis without family. You may also need someone to translate the diagnosis for you, which gives away your privacy,” he said.
For a transition procedure, most specialists require that a trans person get a certificate from a psychiatrist or a mental health specialist stating that they have GID (Gender Identity Disorder) (now referred to as Gender Incongruence or Gender Dysphoria), said Raghuram. “However, general access to psychiatrists is itself limited. In addition, many psychiatrists act as gatekeepers, often based on their own notions of bi-normative and patriarchal gender norms.”
In this Newsminute report, several trans persons revealed that mental health professionals violated their basic right to privacy and were mostly uninformed about gender issues.
Source: The News Minute
‘Family has yet to accept’
Stigma and discrimination can have substantial and complex effects. For instance, Rina said that growing up her parents kept her schizophrenia diagnosis a secret, medicating her without her knowledge. This led to three episodes of psychosis and eventually led her to acquire a physical disability as well, she said without revealing the details of these episodes to maintain her anonymity.
“They have been supportive of the physical disability so far but not so much about my schizophrenia or my gender,” she said. “Any aberration they see in my behaviour is immediately attributed to schizophrenia and I am immediately asked if I had taken medicines or not.”
When Rina came out to her parents 10 years ago, they panicked. The family has yet to accept her gender identity and fear that her disability will not allow her to live as a woman. “For a long time, they used to think that schizophrenia is causing me to think this way,” Rina added.
“Slowly that thought is fading away but I have had to transition and detransition and retransition three times in these 10 years because of their handling of my psychosocial disability,” she said. (Detransition and retransition are the processes of reversing or halting gender transition through social, legal or medical means. Like transition, it is not a single mode/event.)
Financial issues with affirmation surgeries
Many affirmation surgeries are also inaccessible because of the costs involved in the surgery, insurance coverage and other miscellaneous expenses. For those who are disabled and already dealing with medical expenses, these costs could make an affirmation surgery unaffordable.
In 2014 NALSA judgement, the Supreme Court issued directives to Central and state governments to ensure the overall development, equality, and safety of transgender persons in society. After this, Assam, Tamil Nadu, Kerala, Andhra Pradesh, Telangana (Transgender Community Desk), Gujarat, Bihar and Maharashtra among other states set up welfare boards for their formal education, employment, ensure health coverage and legal help to the community with varying impact. But discrimination continues in how trans persons access healthcare, we have reported.
Further, The Transgender Persons (Protection of Rights) Act, 2019 mandates public healthcare provisions, including sex reassignment surgery (SRS) and hormonal therapy, for transgender persons. The Act also recommends the publication of a health manual for SRS in accordance with the guidelines issued by World Professional Association for Transgender Health (WPATH), a network that promotes high standards of care for the health of transsexual, transgender, and gender nonconforming people.
“Some people experience gender dysphoria at such a level that the distress meets criteria for a formal diagnosis that might be classified as a mental disorder,” say the guidelines. “Such a diagnosis is not a license for stigmatisation or for the deprivation of civil and human rights.” It further adds that “a disorder is a description of something with which a person might struggle, not a description of the person or the person’s identity”.
Based on several trans persons’ experiences, BehanBox reported that the entire surgery at a private facility costs somewhere between Rs 2-6 lakh. In several states, access to affirmation surgeries is largely absent. Hormonal therapy, which is a continuous process, costs around Rs 500-800 per month.
Aryan Somaiya, a trans man who underwent a top surgery in November 2021, broke down the costs in an Instagram video: this included travel, lodging and food expenses for at least 18-20 days. Then there are blood tests, HIV, liver functioning, and CBC tests before the surgery, which costs somewhere around Rs 5,000. A consent letter, framed as an affidavit, costs around Rs 700-800. The surgery itself cost him Rs. 1.19 lakh, every post-surgery visit Rs. 1000 and two binder (dressing) sessions Rs. 2000.
No comprehensive forum for interaction
In 2019, to further the rights and welfare of the transgender community, the government enacted the Transgender Persons (Protection of Rights) Act, 2019 and Rules, 2020 or The Transgender Act. It aims to end discrimination against transgender persons in access to education, employment and healthcare. The Act also recommends the publication of a health manual for sex reassignment surgery in accordance with the guidelines issued by WPATH. But neither this act, nor the Rights of Persons with Disabilities Act of 2016, address those at the intersection of disability and trans identity.
Activist Shampa Sengupta further pointed out that there have been few studies on the subject and this constrains the capacity of communities and health service organisations to respond appropriately to the needs, experiences and realities of trans people with disabilities.
Sangath’s Raghuram traces the problem to the lack of updated content on dealing with trans persons or trans persons with disabilities in medical education. As a doctor, he says that he has not witnessed a single discussion in medical schools on how to deal with trans persons with disabilities in his medical training.
What is lacking is a forum where the medical fraternity interacts and consults with trans persons and trans persons with disabilities, said Aqsa Sheikh. “Also, one needs to understand that the interventions cannot be guided by return on investments, but by how ethical and inclusive the services are,” she said.
Campaigning for greater acceptance, support
Nayak feels that his gender identity and disabilities leave him at a crossroad, unable to fully belong to either community. “There is barely any acknowledgement of people who fall at the intersection of disability and trans identity. In organisations working for disability, they don’t talk about trans persons and in trans organisations, they don’t talk about disability,” he pointed out.
In 2008, Nayak started two organisations to foreground the issues of trans persons. His forums are now demanding free counselling, free gender affirming surgeries and hormonal injections in three states — Karnataka, Andhra Pradesh, and Telangana – but their cause has found little support even in the health sector.
“While people offer to help with wheelchairs and aids to deal with disability, they do not talk about our gender or our body in respect to it,” he said. At several meetings with the Telangana state government, he said he had to deal with ignorant questions from ministers: “Who is a transman?” or “How do you become a transman?”
“They are aware of trans women, but are unwilling to accept a transman,” Nayak pointed out. “Government officials do not believe I am a trans man with a disability, they accept my disability but not my gender. Aren’t we humans?”
*Names have been changed to protect identities.
[This is the seventh report on the series on violence and exclusion faced by women and trans persons with disabilities in India as part of the Spotlight Media fellowship. The fellowship is a collaboration between Rising Flame and BehanBox. You can read the previous reports here, here, here, here, here and here.]
Our Newsletter
Subscribe to Our Newsletter
We believe everyone deserves equal access to accurate news. Support from our readers enables us to keep our journalism open and free for everyone, all over the world.